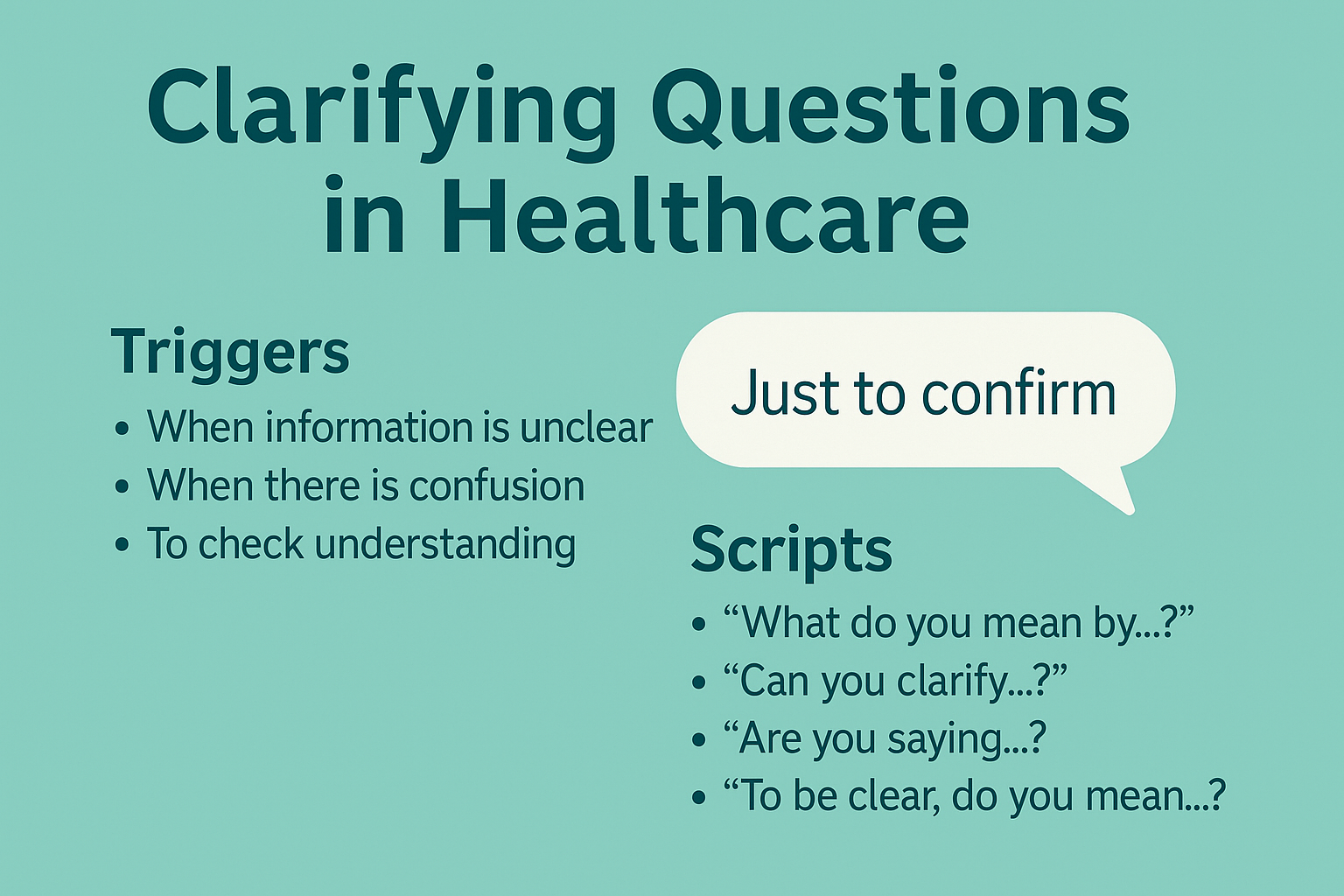
Clarifying questions healthcare practices are the fastest way to catch ambiguity before it turns into a near miss or an adverse event.
One well-timed question—asked without hesitation—can correct a wrong dose, stop a mismatched order, or prevent the wrong site from being prepped.
This guide explains why clarifying works, when to ask, exactly what to say, and how to hardwire the habit into daily routines so your team benefits on the very next shift.
- Why clarifying questions healthcare changes outcomes
- High-yield triggers for clarifying questions healthcare
- The playbook: scripts for clarifying questions healthcare
- Where to hardwire clarifying questions healthcare
- Coaching the habit in 10 minutes a day
- Handling friction without drama
- Making it stick: design cues for clarifying questions healthcare
- Examples that resonate (use or adapt)
- Quick reference: clarifying questions healthcare pocket script
- Rollout plan for the next 7 days
Why clarifying questions healthcare changes outcomes
When workloads spike, people fill in gaps with assumptions. Ambiguity creeps in through sound-alike drug names, fragmented chart notes, and verbal orders in noisy areas. Clarifying questions healthcare interrupts that drift.
The moment you pause to ask “Do you mean IV push over five minutes or a 30-minute infusion?” you transform a vague instruction into a safe, verifiable action.
This tiny exchange reduces cognitive load, aligns mental models, and creates a documented trail that supports safe escalation.
Clinically, the value shows up as fewer label errors, faster escalation on deteriorating patients, and tighter handoffs. Culturally, it builds psychological safety: when asking is normalized, everyone feels responsible for accuracy, not just speed.
High-yield triggers for clarifying questions healthcare
Think of these as green lights to speak up. If any are present, ask.
- Digits and doses: unusual strengths, leading/trailing zeros, weight-based calculations, or ranges (“give 5–10 mg”).
- Route or rate unclear: “IV vs. PO,” “bolus vs. infusion,” or unlabeled pump settings.
- Look-alike/sound-alike items: hydralazine vs. hydroxyzine, dopamine vs. dobutamine, LASA storage.
- Timing conflicts: pre-op NPO vs. med schedule, anticoag timing around procedures.
- Identity/site/side ambiguity: similar names in the same bay; right vs. left; wrong chart open.
- Handoff contradictions: note says one thing, orders say another.
- New device or workflow: temporary workarounds, newly rolled-out order sets, or policy changes.
- Fatigue or interruptions: multiple call-ins during med compounding, night-shift handoffs, alarm floods.
If you recognize one, treat it as a requirement to clarify, not a personal judgment about a colleague’s instructions.
The playbook: scripts for clarifying questions healthcare
These short lines are designed for speed. Pair the question with a repeat-back so the sender hears exactly what you will do.
Confirm the action
- “To confirm, you want morphine 2 mg IV push over five minutes, correct?”
- “I heard CTA chest with contrast now—am I missing any prep?”
Disambiguate numbers
- “Is that one-five (15) milligrams, not five-zero?”
- “Potassium is 3 point 1—repeat, 3.1—shall we replace per protocol?”
Clarify route/rate
- “Do you mean IVPB over 30 minutes or a bolus?”
- “Order says 1 mcg/kg/min—confirm the per minute is intended?”
Identity, site, side
- “Before we prep, can you confirm left forearm versus right?”
- “Two patients named Chen in 4B—this is Wei Chen, 04/04/78, correct?”
Close the loop
- “I’ll document: ceftriaxone 1 g IV at 14:00, then repeat-back when hung—okay?”
Using ARCC (Ask, Request, Concern, Chain of command) helps when pushback happens: Ask a question, Request a pause, state your Concern, and, if unresolved, use the Chain of command.
Where to hardwire clarifying questions healthcare
You’ll get the biggest returns by baking prompts into the places ambiguity shows up most.
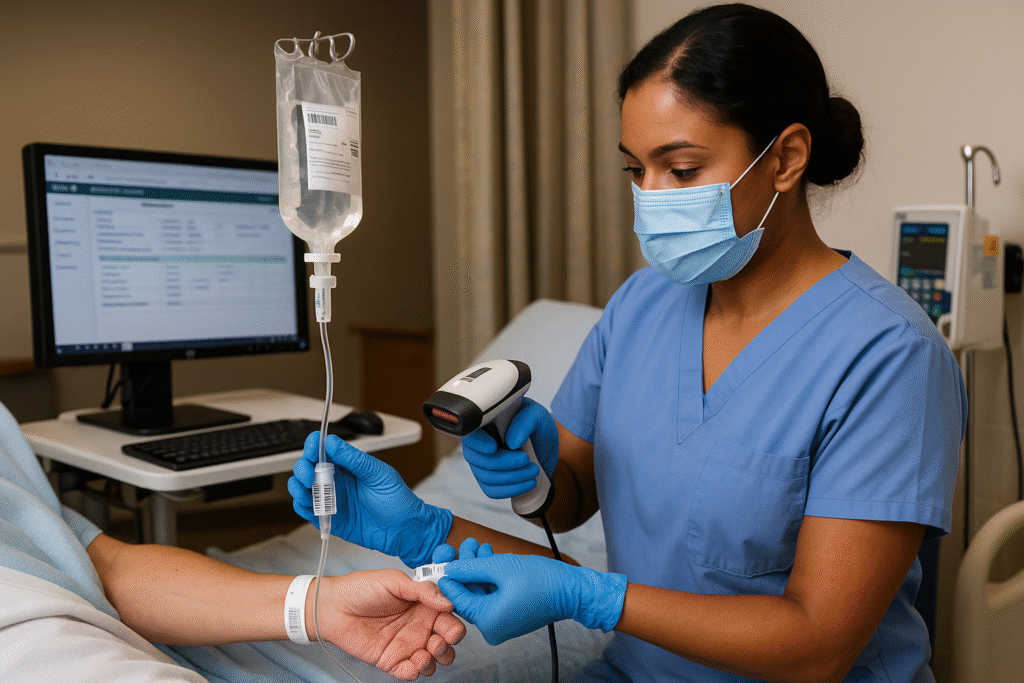
Medication administration
Place tiny prompts at the med cart: “Dose—Route—Rate—Repeat-back.” Add a barcode scan gate that requires entering route and rate in clear fields, not free text. Combine with a quick SBAR one-liner when paging.
Imaging & procedures
Add a single line to requisitions: “Clarified for: study type, side/site, contrast (Y/N).” In pre-procedure time-outs, call on the most junior person to state what they believe is happening; it surfaces hidden confusion.
Handoffs and consults
During SBAR, expect one clarifying question from the receiver and one from the sender. This normalizes the behavior and prevents “FYI” handoffs. Link to your SBAR handover scripts so people see examples.
Daily safety huddles
On your board, add a tiny “Ask to be sure” tile under Today’s Risks. When someone shares a near miss that was prevented by a question, recognize it publicly. If you run huddles, this fits cleanly into your safety huddle template.
Coaching the habit in 10 minutes a day
Teaching clarifying questions healthcare doesn’t require a big rollout—just steady reinforcement.
Model it visibly
Leads ask one clarifying question in each rounding conversation. Announce you’re doing it to set a norm: “I’m practicing one clarifier per handoff.”
Pocket cards and wall cues
Print a one-page card with: digits script, route/rate script, identity/site script, and a phonetic alphabet panel (Alpha, Bravo, Charlie…). Keep it on the badge reel and at the workstation.
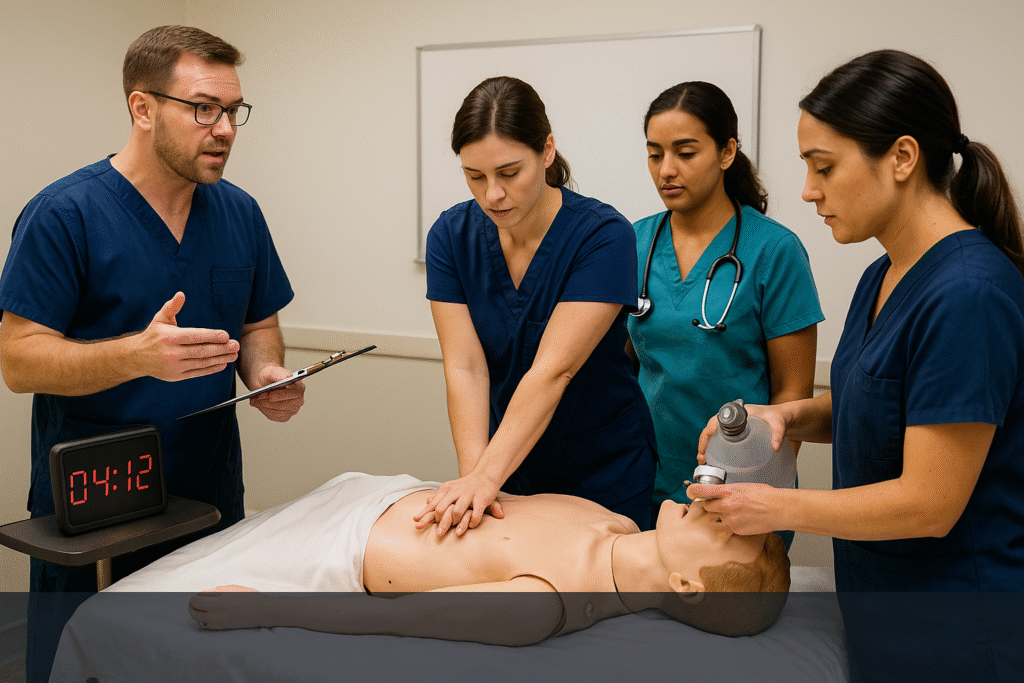
Micro-drills
Run 5-minute simulations of ambiguous orders. Score for one clarifier + repeat-back within 15 seconds. Debrief with 5:1 feedback—five positives for every coaching note—to keep learning safe.
Track two simple metrics
- % of high-risk steps where a clarifier + repeat-back was observed.
- of near misses attributed to clarifying questions (expect a rise early, then stabilization as hazards are designed out).
Handling friction without drama
Occasionally, clarifying sounds like second-guessing. Reduce friction by staying specific and neutral.
- Focus on the action, not the person: “To prevent delay, I want to confirm the dose and route.”
- Use we language: “Can we STAR this step and verify rate before we connect?”
- Anchor to policy: “Our protocol asks us to repeat numbers, so I’ll say it back.”
- If resistance persists, move up ARCC quickly and respectfully.
Psychological safety grows when people see clarifiers welcomed rather than punished. That’s the leadership moment: protect the behavior in public, even if you discuss efficiency privately later.
Making it stick: design cues for clarifying questions healthcare
Form fields that force clarity
Replace free-text with dropdowns for route and unit, and require a decimal guard for doses (no trailing zeros, leading zeros mandatory).
Visual controls
Separate look-alike/sound-alike vials with bold labels and tall dividers. Post a mini chart of LASA pairs at the ADM screen.
Sterile cockpit windows
Create 2–3 minute no-interruption blocks for compounding, order entry, or chemo double-checks. A well-timed clarifier is easier when the environment isn’t noisy.
Standard language
Adopt a unit-wide script: “I’m clarifying…” + repeat-back + “Is that correct?” Consistency beats creativity here.
Examples that resonate (use or adapt)
- Wrong route averted: A verbal “push” order was clarified to “infuse over 30 minutes” after the nurse asked, “IV push or infusion?”—preventing chest discomfort in a cardiac patient.
- Wrong patient prevented: Two similar names; tech asked, “Confirm full name and DOB,” caught a chart mismatch, and avoided a mislabeled specimen.
- Rate error caught: Pharmacist repeated, “One mcg/kg/min—confirm per minute, not per hour?” The prescriber corrected the unit immediately.
Each story took less than 15 seconds. Each protected a patient.
Quick reference: clarifying questions healthcare pocket script
- Numbers: “One-five, 15 mg—confirm one-five, correct?”
- Route/Rate: “Clarifying route and rate: IVPB 30 minutes, not push?”
- Identity/Site/Side: “Confirm left knee for injection on Kim, 02/17/79?”
- Close the loop: “I’ll document and read it back before starting.”
For additional background on building reliable communication systems, see concise primers and tools from the Institute for Healthcare Improvement, the AHRQ Patient Safety Network, and resources on high-reliability from The Joint Commission. These provide practical context you can adapt locally.
Rollout plan for the next 7 days
Day 1: Print the pocket card and post a tiny reminder near the MAR: “Question + Repeat-Back.”
Day 2–3: Ask one clarifier per handoff; keep notes on what felt awkward.
Day 4: Add the phonetic alphabet to requisition desks and phones.
Day 5: Launch a 5-minute clarifier drill at the start of each shift.
Day 6: Share one success story at the huddle; recognize the person publicly.
Day 7: Start tracking the two metrics above on the safety board.
Small habit, big effect. Normalize clarifying questions and you’ll watch uncertainty—and incident rates—fall together.

No comments yet