SBAR handover is the fastest way to make handoffs clear, complete, and actionable—without adding meeting time or paperwork.
When teams consistently frame updates as Situation, Background, Assessment, Recommendation, information travels in the same order every time, cognitive load drops, and decisions speed up.
Below you’ll find seven ready-to-use SBAR handover scripts for common clinical scenarios, plus coaching tips, pitfalls to avoid, and a one-page quick reference you can print for your unit.
- Why SBAR works (and why it sticks)
- The rules of a crisp SBAR handover
- The 7 SBAR handover scripts you can use today
- How to coach SBAR handover in under 10 minutes per day
- Common SBAR handover pitfalls (and quick fixes)
- One-page SBAR handover quick card (copy/paste to print)
- Getting started this week
Why SBAR works (and why it sticks)
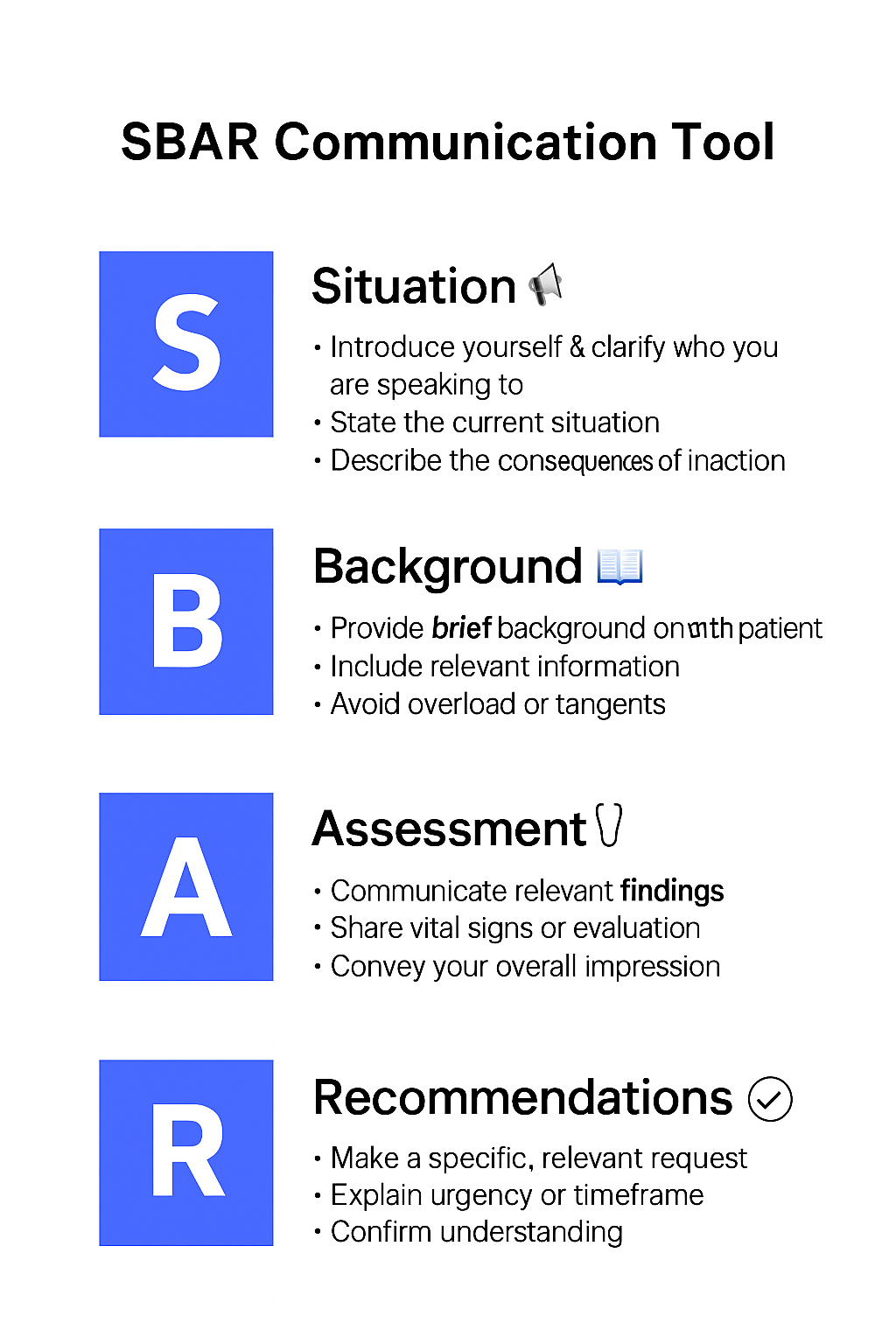
A great SBAR handover does three things: it puts the most important fact first (S), adds only the context that changes decisions (B), states a point-of-view rather than a data dump (A), and ends with a specific ask (R).
Because the structure never changes, the receiver learns exactly where to listen for what—like hearing verse, chorus, bridge in a familiar song.
That predictability is what makes SBAR handover so reliable in busy, noisy environments.
The rules of a crisp SBAR handover
- One breath for Situation. Lead with what is happening now and the consequence if we do nothing.
- Only relevant Background. If it does not alter today’s decision, it belongs in the chart, not the handover.
- A real Assessment. “Looks uncomfortable” is not enough; include vitals or exam that justify the concern.
- Close with a Recommendation. Propose the next step and a time frame; silence invites drift.
Checkout more templates from https://templatelab.com
The 7 SBAR handover scripts you can use today
Each script is written so you can read it verbatim, then adapt it to your local pathways and order sets.
1) Deteriorating patient (rapid response trigger)
S: “This is 4E Bed 12. SBAR handover for Mr. Lopez: sudden hypotension to 82/46 with new confusion.”
B: “Post-op day 1, knee arthroplasty; history of HTN, no bleeding risk meds; urine output falling the last 2 hours.”
A: “Likely hypovolemia vs. occult bleed; skin cool, cap refill delayed; Hgb last 10.2, trend unknown.”
R: “Request rapid response at bedside now, STAT CBC and lactate, 500 mL balanced crystalloid; if no response, plan for MD evaluation for possible transfer.”
Coaching tip: Say the danger in the first sentence. Your SBAR handover should instantly tell the listener why to act.
2) Pain rescue (post-op or trauma)
S: “SBAR handover for Ms. Chen in 3C: severe pain 8/10 unrelieved by scheduled analgesia.”
B: “Post-op day 0 after laparoscopic chole; vitals stable, tolerating sips.”
A: “No red flags for bleed or infection; guarding at incision; non-pharm tried (splinting, heat).”
R: “Request rescue order: hydromorphone 0.2 mg IV q10 min PRN up to 3 doses, plus ondansetron 4 mg IV once. Reassess in 30 minutes.”
Coaching tip: End with one concrete regimen so the receiver can approve or modify.
3) Suspected sepsis (early recognition)
S: “SBAR handover for Mr. Ortiz: febrile to 39.2°C with HR 124 and MAP 62.”
B: “Recently started on ceftriaxone for UTI; diabetic; last creatinine 1.9.”
A: “Meets sepsis criteria with hypotension and suspected source; lactate pending.”
R: “Start sepsis bundle now: fluid bolus 30 mL/kg, broad-spectrum per pathway, blood cultures ×2 before antibiotics; request provider at bedside within 10 minutes.”
Coaching tip: When pathways exist, name them. Protocol cues speed agreement.
4) Imaging clarification (prevent wrong test/wrong side)
S: “SBAR handover for outpatient imaging order: CT chest without contrast was entered, but the note mentions PE rule-out.”
B: “Patient has normal renal function; no contrast allergy on file.”
A: “For PE rule-out, CT angiography with contrast is indicated.”
R: “Please modify to CTA chest with contrast and confirm urgency—STAT or routine?”
Coaching tip: Use the SBAR handover to prevent silent assumption errors. Ask for the one change needed.
5) Medication safety (look-alike/sound-alike)
S: “SBAR handover for medication verification: order for hydralazine 10 mg IV is on the MAR; vial in ADM bin is hydroxyzine 10 mg/mL.”
B: “Patient hypertensive to 186/98; needs IV agent.”
A: “Look-alike/sound-alike risk; wrong drug could cause sedation rather than control BP.”
R: “Request verification of the order and stock; please place hydralazine in a separate bin and add an alert to prevent selection error.”
Coaching tip: Pair the risk with a system fix in the Recommendation.
6) Consult request (clear, concise)
S: “SBAR handover to surgery consult: 67-year-old with peritonitic abdomen and free air under diaphragm on upright film.”
B: “History of PUD; on NSAIDs; NPO since midnight.”
A: “Perforated viscus likely.”
R: “Request surgical evaluation at bedside now; we’ve started broad-spectrum antibiotics and two large-bore IVs.”
Coaching tip: For consults, your Assessment should be a one-line diagnosis, not a maybe.
7) Discharge readiness (get to “yes” or “no” fast)
S: “SBAR handover for Ms. Patel: clinically stable and ambulating independently; asking about discharge today.”
B: “Community support arranged, home meds reconciled; last labs WNL; follow-up booked in 3 days.”
A: “Medically ready pending pain plan and antiemetic rescue.”
R: “Request discharge today with oral analgesic step-down, PRN ondansetron, and return precautions; can we place the orders by noon?”
Coaching tip: Time-box your Recommendation so tasks land on someone’s calendar.
How to coach SBAR handover in under 10 minutes per day
- Pick one script per shift. Announce the day’s focus in the huddle (e.g., “We’re practicing sepsis SBARs”).
- Observe two handovers. Use a micro checklist: S present? B relevant? A argued? R specific and time-bound?
- Give 5:1 feedback. Celebrate strong S and R; tighten B if it drifts into storytelling.
- Standardize the prompt. Embed SBAR handover fields in your handoff sheet or EHR message template.
- Close the loop. End of shift: one example of a handover that led to a fast decision or prevented a mistake.
For concise overviews and examples you can adapt, see primers from AHRQ PSNet and practical guides at the Institute for Healthcare Improvement.
For broader reliability concepts that support SBAR handover, The Joint Commission’s high-reliability resources are also helpful starting points: The Joint Commission.
Common SBAR handover pitfalls (and quick fixes)
- Background sprawl. If your SBAR handover is longer than 60–90 seconds, B is probably bloated. Keep comorbidities only if they change today’s choice.
- Missing Assessment. “FYI” is not an A. Choose a diagnosis or two strongest differentials and state why.
- No ask. End every SBAR handover with a specific action and timeframe; otherwise the receiver assumes you’re just updating.
- Vague vitals. “Stable” isn’t data. Include the one or two numbers that prove your point.
- Unclear urgency. Say “now,” “within 10 minutes,” or “today”—not “soon.”
One-page SBAR handover quick card (copy/paste to print)
S – Situation (10 sec)
- The one-line problem now + risk if nothing happens.
- “I’m calling about… because…”
B – Background (20 sec)
- Only context that changes decisions: diagnosis, critical labs, treatments tried, allergies.
A – Assessment (20 sec)
- What you think is happening + the one or two facts that justify it.
R – Recommendation (10 sec)
- The action, dose, order, or evaluation you want + when.
- “I recommend… within…”
Place this card on your report sheet, rounding clipboard, or unit whiteboard. Pair your SBAR handover with closed-loop communication (“I’ll repeat that back…”) and a quick STAR pause before irreversible steps. If you’re building a whole program, see our related guides: Error Prevention Toolkit, Safety Huddle Template, and Clarifying Questions Cheat Sheet.
Getting started this week
- Today: Print the quick card and choose two scripts to rehearse at the huddle.
- Tomorrow: Add an SBAR handover template to your paging or secure-chat tool.
- By Friday: Audit five handovers for S/B/A/R quality; share one success story where SBAR handover accelerated care or prevented a miss.
FAQ
How long should a good SBAR handover take?
About 60–90 seconds. If it’s longer, trim Background or move details to the chart.
Can non-clinical staff use it?
Yes. Bed placement, imaging, transport, and pharmacy all benefit from a shared SBAR handover structure.
What if the receiver is rushed?
Lead with Situation and your Recommendation. If they agree, you’ve saved time; if not, they’ll ask for the Background they need.

No comments yet